To be obese or not to be
In this section for submissions by our Fellows, Professor Peter Shepherd FRSNZ of the University of Auckland challenges mainstream understandings and approaches to solving obesity.
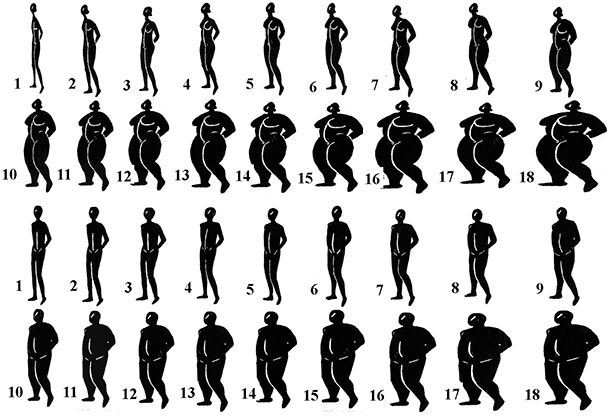
Obesity is one of the most emotive issues of our time, with sensationalist images of obese people, people standing on scales and pictures of piles of unhealthy food used commonly as click bait in our media. It is once again in the spotlight in New Zealand due to recent statements made by senior politicians. It is true that the average body size has increased over the last 30 years which is an issue of medical importance as it is associated with increased risk of diseases such as type-2 diabetes and heart disease. While it is desirable to reduce levels of body fat, body size continues to grow across the world despite intense efforts to develop strategies to reverse this trend. Why have these efforts been unsuccessful?
One part of the reason for this is that people have not looked holistically at the problem and have ignored the biology of obesity. Rather, people have looked to simplistic solutions that at face value sound like they will work, one such view being that this is a matter of “personal responsibility”. This “fat shaming” approach is one that has been used for many years and while it might score political points with some, it hasn’t worked in reducing obesity levels overall. In fact, it can have serious social and psychological effects on those being targeted and it is amazing that it is still tolerated in an age when society has moved to redress so many other prejudices based on moral or societal judgement. These issues are particularly important for Māori and Pacific peoples as rates of obesity (as defined by current ways of measuring it) are higher in these communities.
One major confounding issue is how we define obesity. Medically, obesity is an excess of fat tissue but we don’t routinely measure the amount of fat tissue directly, rather we use the body mass index (BMI) metric as a surrogate. This is because BMI is easy to measure. At a whole population level this does correlate with the levels of fat and since medical systems require simple diagnostic categories it was agreed that, on average, people with a BMI of 30 have a dangerous level of fat in their body. However, these studies were largely done in Europe and America. It is now known that the amount of fat in the body relative to BMI varies greatly in different populations across the world and also within individuals in a given population. In many Asian countries the levels of dangerous fat are observed at BMI’s substantially less than 30 and for Māori and Pacific peoples the BMI at which people have dangerous levels of fat on average is higher than 30. Even within populations the amount of fat vs BMI varies greatly between individuals. The flaws in the one-size-fits-all approach to using BMI are shown by the often quoted example of many All Blacks having a BMI over 30 but clearly not being obese. While the use of BMI is helpful for understanding obesity from a broad public health perspective, to medically address obesity in individuals properly we need more accurate ways of defining what the levels of fat are in individuals.
One reason that the issue of obesity is so controversial is that it seems so simple to be able to lose weight as any difference in our body size is the difference between the amount of energy ingested minus the amount of energy expended. The alarming talk about obesity in the media would have you believe that people's weights are exploding, but in reality our body size does not fluctuate much at all over the short term and obesity develops slowly over long periods of time. This slow rate of obesity development is amazing as we live in an environment where energy dense foods are readily available and where we preserve much more energy by staying much warmer and doing less exercise that we did in previous times. In fact, we tightly control our weight and it has been calculated that the body's ability to achieve a balance between energy intake and energy expenditure (i.e. its set point) needs to be out by only 0.5% for obesity to develop. Again, at face value it seems that it should be such an easy thing to reverse but the reality is that metabolic processes are hard wired into our bodies. Each of us has a set point that corresponds to a weight that is normal for us based on our biology. If we go below this set point our body feels it is under nourished and tries to get us to compensate. This is how we avoid starving to death and explains why voluntary weight loss is so hard for some people as they are fighting their set point. The world is littered with studies that have tried to achieve long term voluntary weight loss through diet and exercise. There are always examples of success for some individuals and these are highlighted as evidence it should work for everyone, but at a population level these dietary weight loss interventions just don’t work over the long term. In saying this, it is important to point out that we should not conflate the potential weight loss effects of exercise with other beneficial health effects of exercise. Exercise should be encouraged independent of any effects on weight loss.
What do we know about the processes controlling our metabolism? We have known for a long time that there is a strong genetic component to body size and shape and this is most obviously demonstrated by the fact that identical twins, who share virtually identical genes, share a very high degree of similarity in height, weight and body shape throughout their lives. In depth studies have even been done on identical twins separated at birth and who lived in different environments growing up and these too share a very high degree of concordance in body morphology. Genome sequencing has added numbers to this and estimates of the genetic contribution to obesity now range from 40 to 70%. Studies from overseas show this genetic component is made up by variations in many genes in European populations, each of which can make a small contribution to metabolic processes regulating body weight. However, we know that in different areas of the world there are differences in overall genetics which means that there are differences in the genes that contribute to this issue. Recent evidence has shown this to be the case with the discovery of a variant in the CREBRF gene found in approximately 25% of Maori and Pacific peoples which is associated with a significant increase in BMI (1.4 BMI units/allele). Surprisingly though this gene variant is associated with a significantly decreased risk of type-2 diabetes and gestational diabetes rather than an increase as might be expected. This shows that it is more complex than it first seems and there is still much to learn about the biological processes controlling metabolism and body shape and size. It also shows we can’t jump to hasty conclusions without really understanding the biology.
So what else has research taught us in the last three decades about how metabolism is so tightly regulated? We now know that two regions in the brain, the hypothalamus and the brainstem, play a crucial role in regulating how much food we eat and how much energy we expend. They act like a computer processing chip to integrate signals that come from sight, smell, taste as well as the signals sent by hormones such as GLP1 coming from our gut, insulin from pancreas, ghrelin from our stomach, leptin from our fat and many others. The outputs not only send signals we are aware of - such as whether we feel full or whether we really want to eat something, but also subconscious signals that act automatically to regulate our metabolism. The integrated sum of these effects our metabolic set point and the differences in our genes dictate exactly where this set point will be in different individuals. We know that it is hard for an individual to alter this set point. However, we are beginning to understand how this knowledge can be used to achieve weight loss reductions in the face of the challenges of the modern environment. The most proven medical route to achieve sustained weight loss over the long term though remains bariatric surgery. This has gone from a dark art to an area where intense research has revealed a lot about the mechanisms of action, efficacy and safety of different types of this surgery and the news is that it works and has long term benefits for health. Unfortunately this type of surgery is greatly under funded in New Zealand compared to other life changing types of elective surgery such as knee and hip operations. We also now know though that some drugs can safely promote some degree of weight loss by targeting mechanisms involved in regulating our metabolism. This includes two classes of drugs that target GLP1 signalling and glucose reuptake in the kidney (SGLT2 inhibitors). These have been recently approved by PHARMAC here in New Zealand so we will see some benefit of these here in future years. More developments in this space are in the pipeline.
History has shown us time and again that the development of successful medical interventions and treatments benefits hugely from incorporating learnings from science.
The last few years have seen an exponential increase in our understanding of how our metabolic set points are regulated and how this contributes to obesity and metabolic health. This tells us that this set point is very tightly controlled but can be very different in different individuals, making some people more at risk in the modern environment than others. It is time for politicians to take personal responsibility to acknowledge this and let science play a role in developing solutions rather than reverting to simplistic emotive moral judgements.
