Impact story: Immunotherapy breakthroughs from fundamental research
Researchers are discovering new ways to train or assist the immune system to fend off
cancers and diseases.
“The immune system is so complex, and many molecular and cellular interactions have yet to be understood,” says Professor Ian Hermans (Malaghan Institute of Medical Research).
“But some of the biggest breakthroughs in immunotherapy have come from basic research.”
Hermans is fortunate to have seen the wins that can stem from Marsden-funded research. His group shed important new light on dendritic cells, which play a crucial role in anti-tumour immune responses.
Professor Ian Hermans
Dendritic cells, explains Hermans, “can determine whether an infection has taken place, or if tissues have mutated and become cancerous, and then co-ordinate an appropriate immune response.”
The pioneering work showed how dendritic cells are involved in stimulating the activity of T-cells, which we all rely on to fight off viruses and intracellular bacterial infections. It ultimately contributed to the now widely accepted view that no two dendritic cells are the same, with some being better at the specific task of stimulating T-cells.
“All of this has proven very useful information for designing vaccines,” he says.
For Associate Professor Bridget Stocker (Te Herenga Waka—Victoria University of Wellington), Marsden funding proved pivotal in pinpointing a molecule found to help our bodies mount a more effective immune response to vaccines.
Back in 2014, Stocker was eager to investigate a class of compounds found on the cell wall of M tuberculosis bacteria (the cause of TB), and particularly an immune-cell receptor within them called Mincle.

Associate Professor Bridget Stocker representing the life balance of chemical research and raising four kids.
Throughout a fruitful, decade-long research programme, Stocker and team, in collaboration with Japanese molecular immunologist Distinguished Professor Sho Yamasaki, have shown how activating Mincle makes for a unique immune profile that can be harnessed for a range of vaccination settings.
A US biotech company now has a licence on one of the team’s patents, and Stocker and research colleague, Associate Professor Mattie Timmer (Victoria University of Wellington), are currently working towards vaccine development with the Switzerland-based Vaccine Formulation Institute (VFI), with the goal of getting the adjuvants into the clinic.
Victoria University of Wellington microbiologist Professor David Ackerley can attest to his own Marsden-funded journey from curiosity to success. His research team’s work on NTR 2.0 – a breakthrough tool for studying degenerative diseases – was originally just a minor part of a 2019 Marsden Fund grant.
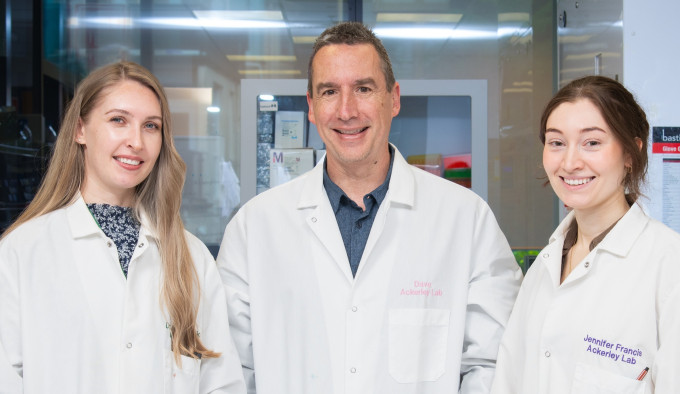
Dr Abby Sharrock, Professor David Ackerley, and Dr Jenni Francis who developed the NTR 2.0 tool for studying degenerative diseases.
The project was originally focused on screening soil DNA to uncover genes that offer weak resistance to antibiotics, tapping into the vast genetic diversity found in thousands of bacterial species.
Using a technique involving a strain of E coli, Ackerley’s team was studying antibiotics including metronidazole, commonly used to treat urinary tract infections and other conditions. When they found E coli wasn’t naturally susceptible to this antibiotic, they turned to an enzyme engineered by another team member, postdoctoral scientist Dr Abby Sharrock. Called nitroreductase, or NTR 2.0, this enzyme allowed the team to create a hypersensitive strain of E coli, making it easier to study genes that could make bacteria resistant to the antibiotic.
They found that the applications for NTR 2.0 stretch well beyond bacteria. In a moment of serendipity, as Ackerley’s team was working on metronidazole, at the same time Professor Jeff Mumm was looking at the drug in his own research at United States’ Johns Hopkins University.
Mumm, whose career has long focused on neuronal regeneration, had already envisaged a clever solution whereby a gene, encoded by an enzyme, could activate an artificial drug like metronidazole.
NTR 2.0 proved the solution that Mumm was looking for, and a study between the researchers found the enzyme could kill targeted cells with much smaller doses of metronidazole.
The team have since deposited their tools in an open-access repository, where research groups can access them for studying degenerative diseases ranging from Alzheimer’s to diabetes.
“Several hundred groups around the world have already accessed these tools, so it’s exciting to think about all the different kinds of degenerative disease research that our work will be supporting.”
He saw NTR 2.0 as a powerful example of what researchers could achieve when enabled by Marsden funding to explore all the “meandering sidelines” of research they were excited and driven by. “Many of those sidelines will lead nowhere, but sometimes, when you have a particular bolt of inspiration from amalgamating ideas, that might be exactly what is needed to come up with a totally new solution to a problem.”
Microbiologist Professor Greg Cook FRSNZ has his own tale of Marsden-funded research leading to exciting opportunities for drug discovery.
An $825,000 grant awarded in 2016 allowed a team led by Cook and his Ōtākou Whakaihu Waka - University of Otago colleague, Professor Kurt Krause, to delve into work that’s helped tackle antibiotic resistance and boost treatments for tuberculosis (TB).
Cook says the TB pathogen, M tuberculosis, is unrivalled in its ability to infect and kill humans – some 10 million people develop TB each year and 5,000 die from it each day – and it’s famously hard to study and treat. But their study, which involved a team of international collaborators including Nobel Prize winner Professor Hartmut Michel, proved a major step forward.

Professor Greg Cook
It described, for the first time, the atomic structure of a key protein called bd oxidase, which lives inside the cell membrane of the TB bacterium and helps it to breathe under the low-oxygen conditions often found in TB-infected lungs. When the team knocked out this protein, they found the drug bedaquiline was able to kill M tuberculosis much faster.
Some new inhibitors have already been identified off the back of the work, with small animal trials now underway in a partnership between Otago and China’s Jinan University, and a global pharmaceutical company that drew on the seminal research for its own inhibitors.
Emeritus Professor Colin Green’s Marsden-Fund seeded science has followed a similar path from discovery to trial. That began in 1997, when the ophthalmologist received a grant for a project focused on antisense oligonucleotides: small fragments of DNA that can bind to specific RNA molecules and stop them from being translated into proteins.

Emeritus Professor Colin Green.
Green’s team at Waipapa Taumata Rau - University of Auckland sought to learn whether these fragments could regulate cell-cell communication through specialised channels known as gap junctions, preventing production of a protein that blocks wound healing.
As Green and colleagues pushed the research further, they found their approach worked by regulating the body’s innate immune system, and that it had more promise for chronic conditions than for the initial target of treating acute wounds. Two drugs, Nexagon and Xiflam, are now in mid or late-stage clinical trials, with the latter being tested against diabetic macular oedema, age related macular degeneration, and long COVID.
“The work has built up more than 100 full research publications and reviews, more than 465 patents worldwide, multiple international collaborations and had added to New Zealand’s research standing on the world map,” Green says. “And the whole story started with fundamental Marsden Fund research.”
- Jamie Morton, 2025.
