Research
Published 11 August 2023Dissecting the link between the Group A Streptococcus, infection, and immunity
In this Marsden Fast-Start, Dr Catherine Tsai from Waipapa Taumata Rau The University of Auckland wants to know how our immune system recognises key parts of Group A Streptococcus and whether this knowledge will help the fight against other diseases
Streptococcus pyogenes (Group A Streptococcus, GAS) is a concerning human pathogen that can cause a wide range of diseases from mild skin infections and sore throats to the more serious and potentially deadly necrotising fasciitis (flesh-eating disease), toxic shock syndrome, and rheumatic heart disease. In Aotearoa New Zealand, these serious complications disproportionately affect Māori and Pacific children with some of the highest rates in the world – between 4 and 7 times higher than New Zealand Europeans for GAS skin infections and acute rheumatic fever. Meanwhile, cases of this severe invasive GAS are continuing to increase in high-income countries around the world.
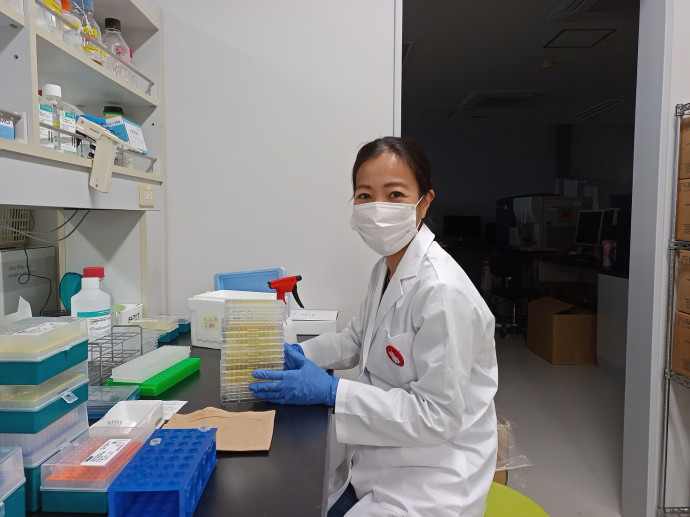
Dr Catherine Tsai in the lab. Photo: supplied
Many bacteria including Streptococcus pyogenes have long, thin, hair-like structures, called pili (singular: pilus), on their surface. These pili are formed by chains of protein subunits that resemble strings of pearls. Due to their important roles in host cell attachment and colonisation, GAS pili are an important virulence factor and also a promising vaccine target. Most information about pili focuses on their structure and function, while their interaction with the immune system has not yet been investigated. Dr Catherine Tsai wants to know how our immune system recognises GAS pili to mount an immune response, and if the immune response contributes to disease severity. Furthermore, Dr Tsai and her team want to find out if we can harness this ability to enhance immune responses stimulated by vaccines, which can potentially fight not only Group A streptococcus, but a host of other diseases as well.
Inflammation is a host defence necessary for combatting infection, however, excessive, and misdirected inflammatory responses can cause damage. Dr Tsai and her team are investigating if different pilus types correspond to different levels of immune response and disease severity. Their approach uses a related but non-pathogenic bacterial species, Lactococcus lactis – a bacterium equally useful in dairy foods production and in science research. The team generated modified strains of L. lactis that each expressed a different type of pilus produced by GAS strains. They will test how well these strains provoke an immune response in human immune cells cultured in a dish and in living wax worms. This specific insect displays an immune response with remarkable similarities to that of mammals, making them a useful alternative to traditionally used rodents, and with the extra benefit of being easier and cheaper to maintain.

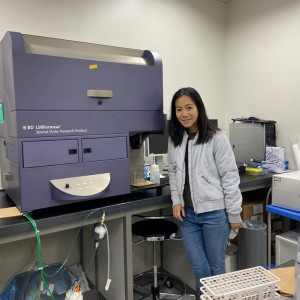
Catherine working with a lab mouse. Photo: supplied
Dr Tsai is also interested in knowing if the immune-stimulating property of GAS pili can be exploited to enhance the efficacy of vaccines. The goal of any vaccine is to stimulate a strong and long-lasting immune response. Thus, Dr Tsai is also testing if GAS pili can be used as a “shuttle” to safely deliver antigens from another disease to our immune systems. An antigen is the part of an invader that our cells recognise and builds antibodies against. So, when the invader next appears, the circulating antibodies quickly identify and attack it, protecting us against that specific disease. In this area of research, Dr Tsai’s team is again using GAS pili grown on Lactococcus to deliver a small antigen. In a separate approach, only specific pilus protein subunits instead of a full pili are being trialled as immune response enhancers (“adjuvant”) and fused with antigens. In a recent trip to Tokyo University and Chiba University in Japan, they tested several prototype vaccines containing influenza A virus antigens in mice. This research is still underway, but they are analysing their results to see if the mice display future protection against influenza A, and which vaccine – pili/protein combination was the most effective.
Combining these two studies, Dr Tsai imagines a future where vaccination against serious disease could be as easy as eating a tub of yoghurt – with friendly, modified Lactococcus bacteria harnessing the power of GAS pili proteins to induce desirable immune responses.
RESEARCHER
Catherine Tsai
ORGANISATION
Waipapa Taumata Rau The University of Auckland
FUNDING SUPPORT
Marsden Fund
CONTRACT OR PROJECT ID
UOA2007: Investigating the Immune Responses to Group A Streptococcus Pili
